Artificial intelligence (AI) based clinical decision support systems (CDSS) are becoming ever more widespread in healthcare and could play an important role in diagnostic and treatment processes. For this reason,

Giorgia Lorenzini
May 5, 2024
Artificial intelligence (AI) based clinical decision support systems (CDSS)
Artificial intelligence and the doctor–patient relationship, expanding the paradigm of shared decision-making.
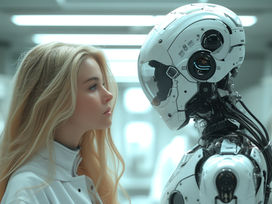
Artificial intelligence (AI) based clinical decision support systems (CDSS) are becoming ever more widespread in healthcare and could play an important role in diagnostic and treatment processes. For this reason, AI-based CDSS has an impact on the doctor–patient relationship, shaping their decisions with its suggestions. We may be on the verge of a paradigm shift, where the doctor–patient relationship is no longer a dual relationship, but a triad. This paper analyses the role of AI-based CDSS for shared decision-making to better comprehend its promises and associated ethical issues. Moreover, it investigates how certain AI implementations may instead foster the inappropriate paradigm of paternalism. Understanding how AI relates to doctors and influences doctor–patient communication is essential to promote more ethical medical practice. Both doctors' and patients' autonomy need to be considered in the light of AI.
It is certainly challenging to introduce AI in healthcare, but this should not be a sufficient reason to desist. While AI may profoundly alter the doctor–patient relationship, this change is not necessarily for the worst since it could further foster SDM, if carefully implemented. However, it should be borne in mind that this will also involve a paradigm shift: while SDM principles may not vary, the fundamental relationship that lies at their core will. Not only could the modes of interaction be altered, but the parties involved will be different as well. As AI is increasingly being implemented, the SDM dual relationship should be redrawn as a triad, involving the patient, the doctor, and the AI. The introduction of AI shifts the medical relationship paradigm to a new form of SDM that is shared between AI, doctors, and patients.
The new triadic SDM relationship should ensure good AI–doctor–patient communication. This could be attained on the hand, by ensuring that doctors have the competence to understand and evaluate AI's outputs while bearing in mind its limitations. On the other hand, patients should be informed of AI's involvement to allow them to better participate in the SDM process. Therefore, decision-making is truly shared when both doctors and patients are in a position to contribute, each with their unique expertise (would this be medical knowledge, contextual clues, empathy, or personal values and preferences), to the final decision, even when an AI is involved.
Including both doctors and patients in the AI decision-making process should guarantee that patients' values and preferences are considered, thus preserving their autonomy and that doctors' professional autonomy is safeguarded. A similar collaborative relationship allows for AI, doctors, and patients to join forces. Eventually, this collaboration could result in better care.
AI
GHBIO
Ethics
Humanity
Presence and Impact